Rectal prolapse (anal prolapse)
The rectum is the last part of the digestive system, and solid waste products leave the human body through the anus.
What is rectal prolapse?
Rectal prolapse is the prolapse of part of the rectal wall or mucous lining out of place or even out of the anus.
Rectal prolapse (anal prolapse) occurs more in young children, older adults and occurs in women over 50 years of age. Rectal prolapse (anal prolapse) also affects young people of both sexes, but at lower rates than adults and children of age.
Types of rectal prolapse (anal prolapse)
Rectal prolapse can be classified into three types:
Partial anal prolapse
Partial prolapse , which is a prolapse of the mucosal prolapse: in which a part of the mucous lining of the rectum comes out from its place, and the lining may slide out of the anus if the intestine is subjected to severe effort, and this condition is common in those affected by Children under two years of age.
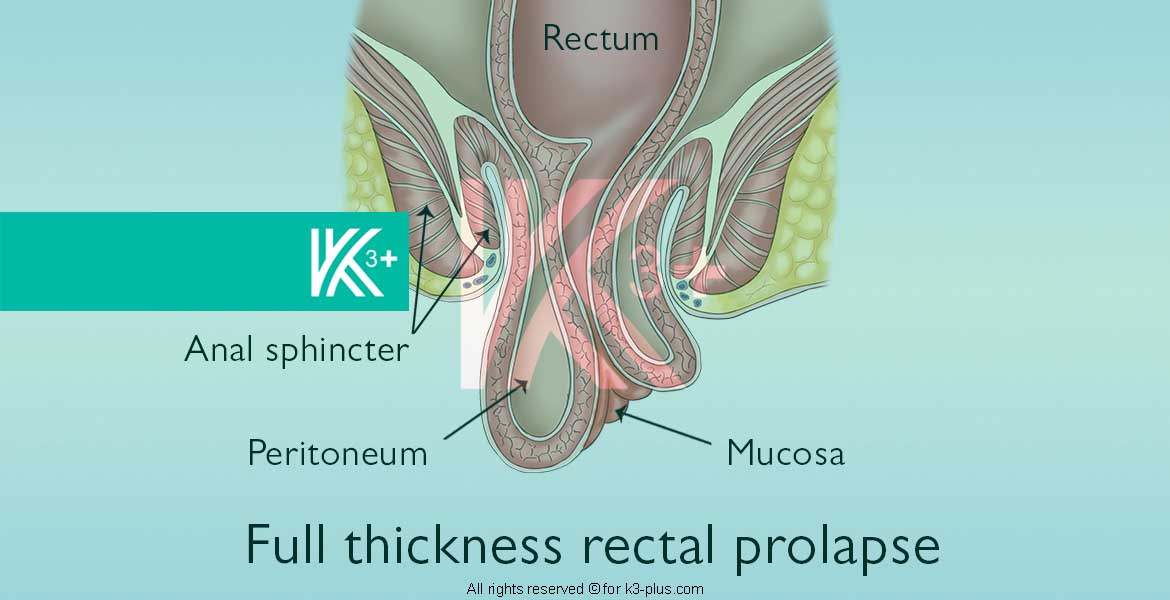
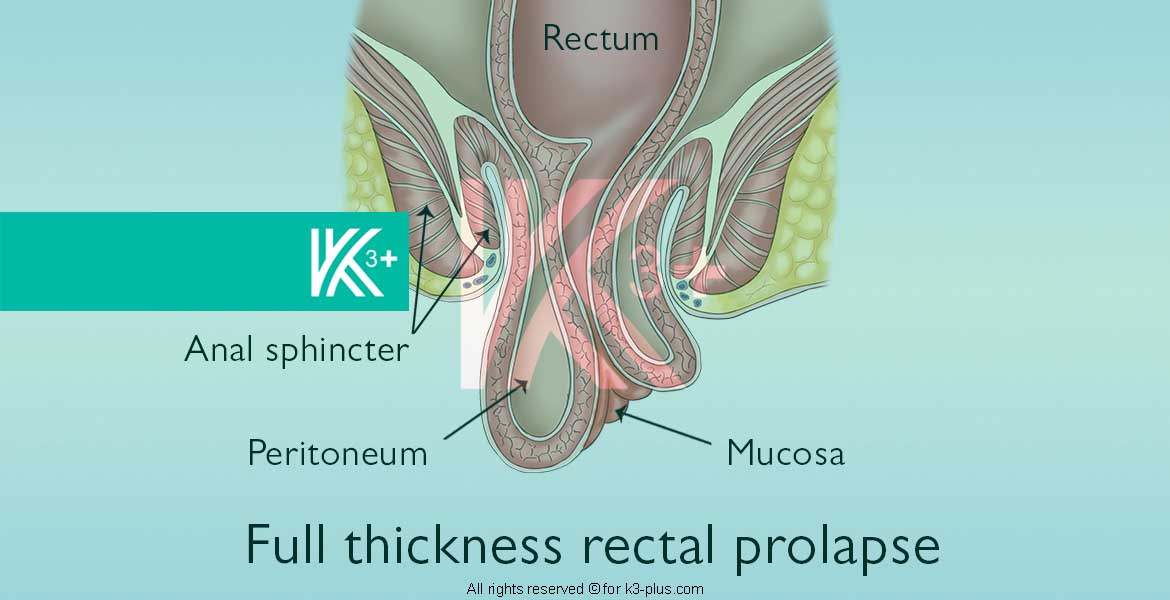
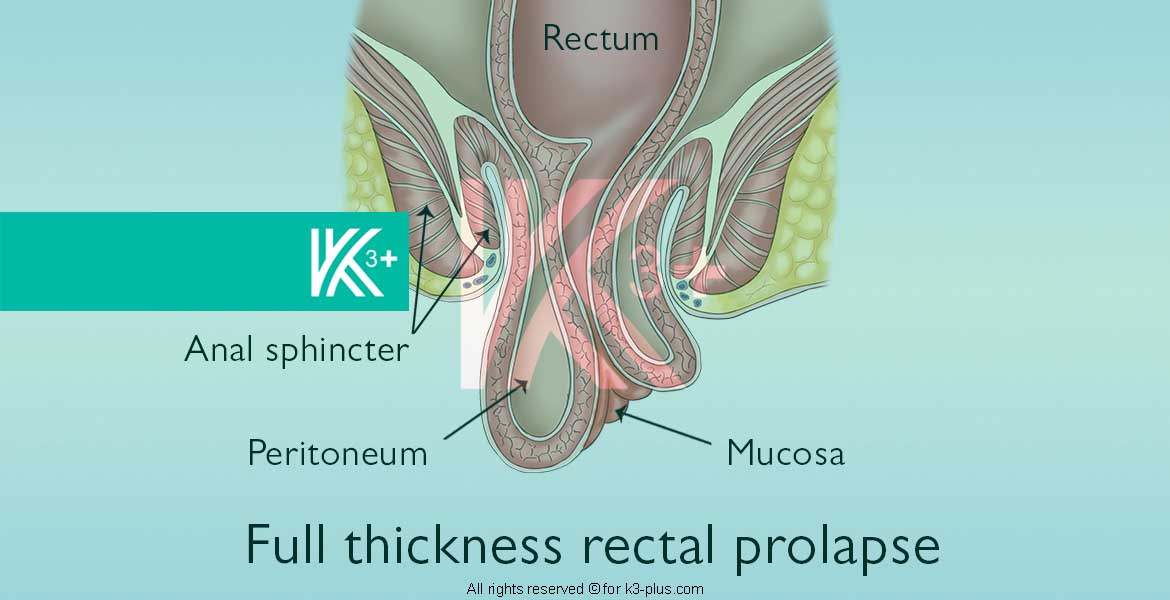
Full anal prolapse
Complete prolapse is the exit of the rectal wall completely from its normal position and can exit outside the anus, this condition begins to appear during defecation and the rectal wall comes out from the anus, then comes out when walking and standing, and then the rectal wall can remain outside Anus all the time.
Internal anal prolapse (intussusception)
Internal prolapse (intussusception) : This is a condition in which parts of the large intestine or rectum are out of place and moved to over other parts and stacked on top of each other, and it is a condition that occurs more often in the elderly and young also, not in young people.
The following is a video by Dr. Khaldoon Al-Gharib talking about rectal prolapse, its diagnosis and treatment:
Rectal prolapse treatment video (with English subtitle)
Symptoms of rectal prolapse
The patient with rectal prolapse loses the ability to control the exit of stool, and suffers from the symptoms of fecal incontinence with a sticky exit from the rectum, and this situation makes the person very confused and gives a feeling of lack of hygiene and the presence of stool that comes out permanently and intermittently and affects daily life.
Difficulty controlling stool occurs in patients with rectal prolapse because the curvatures of the rectum after drooping disappear and the rectum becomes actually straight, which makes controlling and preventing stool from coming out by the muscles is very difficult.
Symptoms of partial anal prolapse
The most prominent symptom of partial rectal prolapse (anal prolapse) is the emergence of a swelling (lump) in the last visible part of the anus or even a lump, at first this swelling appears accompanied by defecation, and the patient’s condition develops to occur with coughing and standing.
Symptoms of complete anal prolapse
The patient may find himself able to push the stuck lump using his fingers, but it is difficult for him to do so, and once he pushes it, he will defecate again, so the patient does not try to push it again. Rectal bleeding and discomfort may occur in the lower abdomen. An ulcer may develop in the prolapsed part of the rectum.
Symptoms of internal anal prolapse (intussusception)
The patient feels the presence of something foreign stuck in the rectum after the stomach empties waste (after a bowel movement).
Diagnosing rectal prolapse
First, the doctor needs a direct physical examination of the rectum (through a sensory examination through the anus). The doctor may be able to diagnose rectal prolapse from a sensory examination, or request a referral to a doctor specializing in digestive diseases, especially intestinal motility.
Tests to diagnose rectal prolapse
The following examinations and tests are performed on patients or those believed to have rectal prolapse (anal prolapse):
Imaging of the rectum
Proctography is a type of x-ray that shows the rectum and anal canal when you have a bowel movement.
Sigmoidoscopy
A sigmoidoscopy is a tiny tube with a camera and a light attached to its end that sees the proctologist and the intestine from the inside.
Colonoscopy
A colonoscopy: A thin, flexible tube with a camera called a colonoscope. The doctor views the inside of the large intestine.
Ultrasound
Ultrasound or endoanal ultrasound is an ultrasound probe for the doctor to see the muscles responsible for and control bowel movement
Differential diagnosis
When trying to diagnose rectal prolapse (anal prolapse) one should consider the presence of any of the following diseases, distinguish their symptoms and their presence:
- Hemorrhoids.
- Intussusception.
- Proctitis.
- Swelling of the rectal mucosa.
Treatment for rectal prolapse (anal prolapse)
The early stages of the disease
The doctor advises to take the following if the disease is diagnosed:
- Eat plenty of vegetables and fruits, and eat foods rich in fiber
- Drink water in abundance to increase intestinal motility.
Dr. also prescribes laxatives such as polyethylene glycol, an osmotic laxative that treats constipation, thus emptying the bowel easily without pressure.
Treating the factors causing rectal prolapse
Treating constipation and diarrhea, often if either of them is the cause, providing supportive care according to the degree of the clinical situation, and in the event that the prolapse of the rectum is irreversible, or has gangrene or a laceration of the rectal mucosa, if there is fecal incontinence, a surgical evaluation should be made according to the case.
Eating vegetables, fruits, and peas frequently helps children with rectal prolapse (anal prolapse) recover without treatment, but consulting a doctor is necessary to regulate their bowel movement.
Sometimes an injection is given with a substance that hardens the hanging parts of the tissue and thus destroys these tissues to be removed.
Rectal prolapse surgery
Surgery is an effective treatment for rectal prolapse, and it is done in two ways, abdominal surgery and perineal surgery. This depends on the sagging tissue itself, the patient’s age, and the rest of the data. The two surgical methods available are:
Abdominal surgery
Through the endoscope, a rectal patch and fixation is placed, and the rectum is raised from the back, up to the coccyx, to the horizontal ligaments of the ends.
Perineal surgery
It is performed for the elderly and those suffering from a serious condition and not tolerating general anesthesia
Immediately postoperative situation
Immediately after surgery, there remains pain in the abdomen and slow bowel movement, so food remains through intravenous fluids until the intestine returns to its normal activity. But it is necessary to adopt a low-fiber diet for a period of 2-3 weeks, and then take fiber supplements, so constipation must be avoided.
Complications following rectal prolapse surgery
Postoperative complications include: infection, bleeding, intestinal injury, changes in sexual or bladder function, and constipation.
Dangerous anal prolapse
The risk of rectal prolapse (anal prolapse) to the child
In the event that a rectal prolapse (anal prolapse) is found in the child, the necessary tests must be performed to ascertain the causes and avoid complications of any of these causes, which may be:
- Cystic fibrosis
- Anal surgeries, especially in children under two years old.
- Malnutrition.
- A deformity or disorder in the development of the body.
- Straining or straining during bowel movements.
- infection.
The risk of rectal prolapse (anal prolapse) for adults
If rectal prolapse (anal prolapse) is found in adults, the necessary tests must be performed to ascertain the causes and avoid complications of any of these causes, which may be:
- Constipation, and the fatigue it causes during bowel movements
- Pregnancy.
- Damage to a part of body tissue as a result of surgery or childbirth.
- The muscles of the basal pelvis are weak and are normal with age
- Chronic enlarged prostate.
- Chronic obstructive pulmonary disease (COPD).
- Cystic fibrosis.
- Pertussis cough.
- Nervous disorders.
- Spinal cord tumors.
Rectal prolapse FAQ
When defecating, I feel part of the rectum drooping out, but I push it in with my finger and it comes back, can my condition improve and stop going down on its own without treatment, and is pushing it useful to stop it?
I feel unable to control the anal muscle since the birth of my son 6 months ago, despite my ability to fully control the excretion of stool and gases, but I feel as if I cannot contract the muscle as before, does this mean that there is a rectal prolapse?
I have a condition that I thought was hemorrhoids, but after reading the description, I think that it is a straight prolapse, can I be sure without visiting the doctor?
I have a straight prolapse and it has been outside the anus by 5 cm a month ago. Can he recover without visiting the doctor, as I see this as embarrassing?
Proctology Cases
Patients who previously lived suffering from hemorrhoids, fistulas, and hair bags, and received treatment by Dr. Khaldoun. We list the symptoms they suffered and the treatment that was provided, which could be useful for you.