Anal Fissure
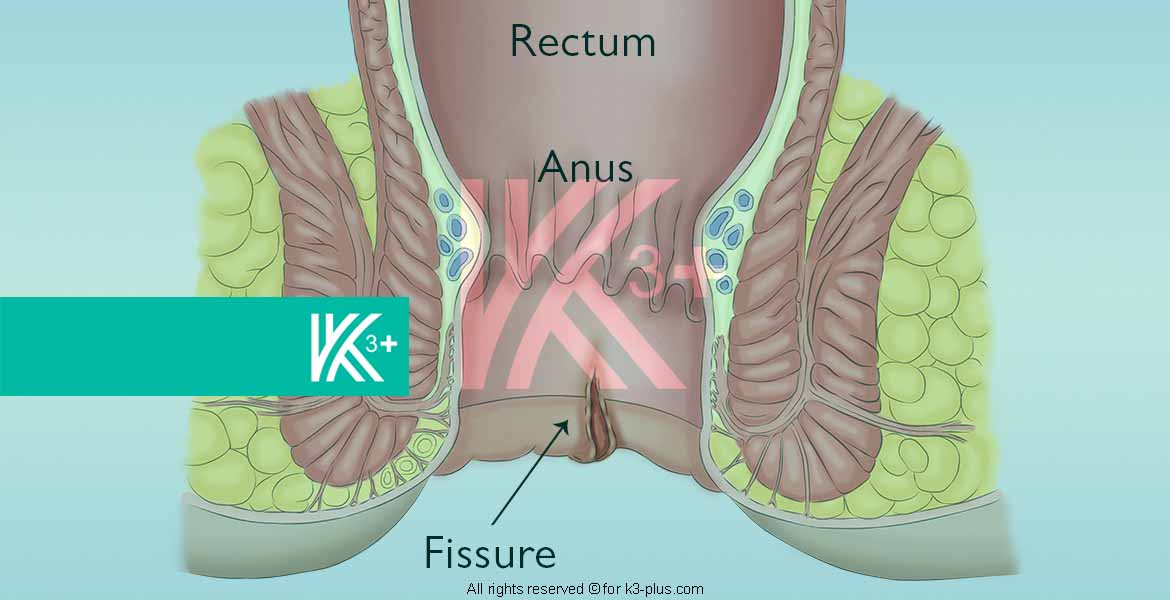
What is an Anal Fissure?
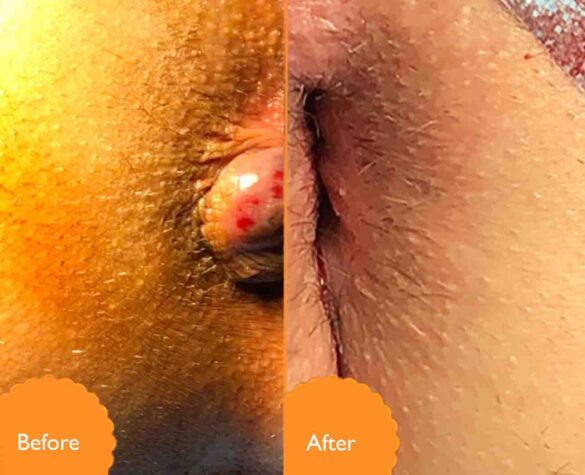
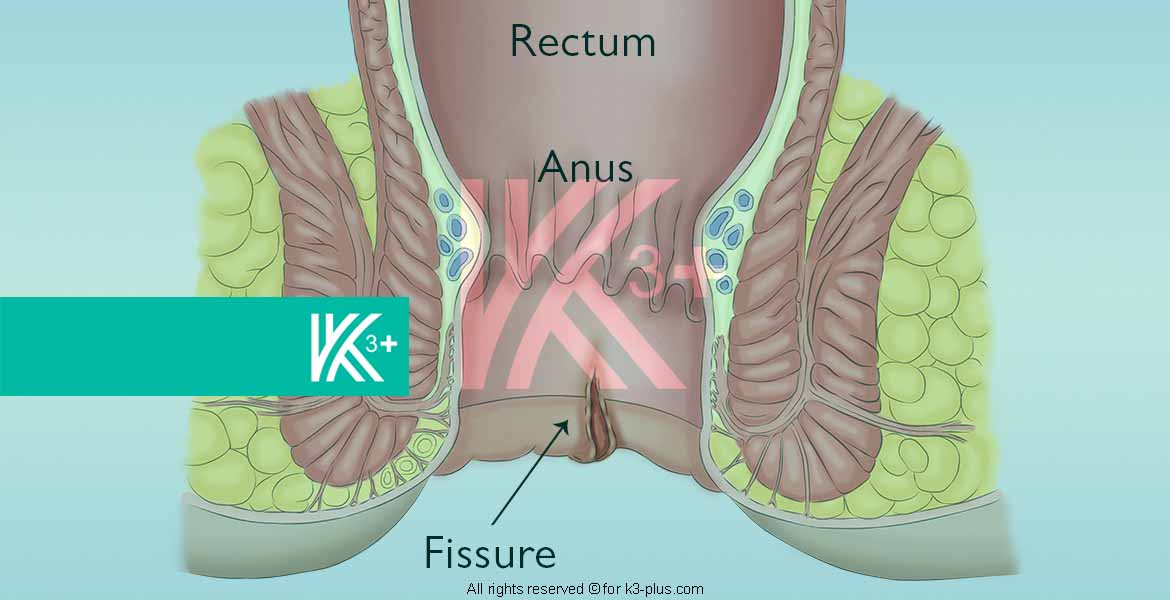
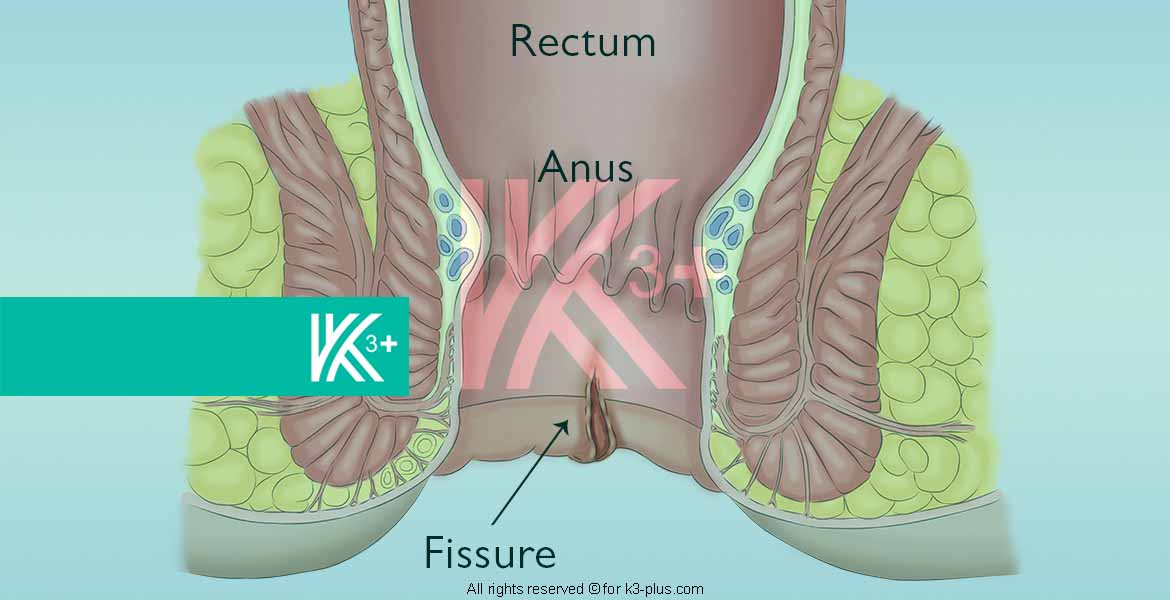
Anal fissures are a common disease in which an opening (wound) occurs in the lining of the anus (under the rectum) and is very painful. It affects all people of all ages and health status, males and females. Hemorrhoids are associated with anal fissures in some cases, noting that anal fissures do not develop into other dangerous diseases such as colon cancer.
Causes of Anal Fissures
The cause of an anal fissure is trauma or damage to the opening and the anal canal, defecation is what causes this trauma most often resulting in the occurrence of the fissure, the patient feels the occurrence of a fissure during defecation even if it is not fully diagnosed, but he realizes the pain and describes it to the doctor, hard stool and diarrhea both cause Anal fissure.
Insertion of a thermometer into the anus, an enema, an endoscope, and an ultrasound probe for examining the prostate glands are all reasons for trauma to the anus that may result in a fissure. Natural childbirth may also cause trauma to the skin between the vagina and the anus in the posterior (perineal region), causing a fissure that extends into the anal canal.
Anal fissures are often located posteriorly (90% of cases) due to the surrounding muscle structure, so the midline of the anal canal from its posterior side is the place where most anal fissures occur, and it is the part closest to the spine than the anus. There is a grouping of muscles (the external and internal anal sphincters) surrounding and supporting the anal canal. These sphincters are oval and have good support on both sides better from the front and back, but the weakest point is on the back side, so the fissure is likely to occur on the back side of the canal epithelium. Anorectal.
The vagina in women weakens the stent at the front end of the anal canal, so the fissure occurs from the front in 10% of cases in women and only 1% in males, with the possibility of the formation of an appendix of skin at the end of the anal fissure called the sentinel nipple.
The occurrence of the fissure in sites other than the anterior and posterior sides calls for suspicion of another condition causing it, such as anal cancer, Crohn’s disease (4% of Crohn’s disease has an advanced anal fissure), leukemia, and several infectious diseases such as tuberculosis and viral infection (CMV (impetigo)) Syphilis, gonorrhea, chlamydia, Haemophilus influenzae (chancroid) and AIDS (human immunodeficiency virus (HIV)). Half of all Crohn’s disease patients develop anal ulceration similar to the anal fissure during the disease stages.
Defecation and Anal Fissure
The natural bowel movement
Studies have indicated that the muscles surrounding the anal canal are spastic (constricted) in patients who suffer from frequent anal fissures, and this results in a higher than normal pressure in the canal. The external sphincter and the internal sphincter flank the anal canal. The first is a striated voluntary muscle that a person can control according to his desire, either by tightening it to prevent the exit of faeces or relaxing it to allow the exit of stool. While the second muscle, which is the internal anal sphincter, is a smooth, involuntary muscle, which cannot be controlled by a person, this muscle is always contracted to completely prevent small amounts of stool from leaving the rectum. But when a large amount of stool reaches the rectum when defecating, the internal anal sphincter relaxes automatically, allowing stool to pass (this happens unless the person voluntarily closes the external anal sphincter), then returns to its normal state of contraction (spasticity) and remains on it Until the next defecation.
Defecation with an Anal Fissure
If an anal fissure has already occurred and immediately after passing out, the internal anal sphincter muscle contracts more than normal for a few seconds, then moves to the resting position, in which it returns to another contraction level, but also higher than normal. As a result, and due to the high pressure and tension of the muscle, both immediately after defecation and also during the resting stage, both lead to pulling the edges of the incision away from each other in a way that opens the wound (the incision) and prevents its healing.
The force of the incoming blood flow towards the anal canal and anal opening also has a role in preventing anal fissures from healing. Several microscopic anatomical studies have indicated that blood flow to the back of the anal canal, where most fissures occur less than to the rest of the anal canal areas in 85% of people.
Also, blood flow in the posterior anal canal is less than half the blood flow in other parts of the anal canal. This helps prevent anal fissures from healing. Also, spasm of the internal anal sphincter increases pressure on the anal canal, thus increasing the pressure of blood vessels on the anal canal and increasing blood flow.
Fissure’s Symptoms
Dr. Khaldoun Explain about Fissure (video includes English subtitle)
- One of the most important symptoms of anal fissures is very acute pain, so the patient often sees the doctor within a few days of the occurrence of an anal fissure, and there are other cases that a person has a fissure and remains for a while without the patient’s awareness of it and thus the fissure is classified as a chronic anal fissure.
The pain is usually stinging during a bowel movement (the pain may last for moments or for several hours after a bowel movement).
In some cases, no pain may be felt. - Burning during defecation.
- Anal itching.
- Bleeding; The crack often leaves a small stain of bright red blood on the toilet paper. Therefore, it is necessary to inform the doctor. It is also necessary to distinguish the location of the blood and its color
- Blood separated from stool, clear color, and other things necessary to inform the doctor about it.
- Blood mixed with stool is usually a sign of another condition that could be enteritis or colon cancer
Note: An anal fissure may not cause any pain for some people, but it remains without healing and bleeds intermittently and does not show any other symptoms with it.
Examinations and tests
Anal fissure is diagnosed by a doctor, a clinical examination is done and the symptoms are known, and the examination may include the following:
- Inspection of the incision by gently dividing the buttocks and looking
- Touching the rectum with a finger. It feels the structure of the anal canal after wearing gloves.
- Anoscopy. Through a short-range lighted endoscope to look inside the anal canal
The finger examination and anoscopy are usually performed by the doctor after the fissure begins to heal, but if the examination is necessary immediately, this can be done with local anesthesia of the area.
The diagnostic stage includes knowing:
- Number of slits; Is it one slit or more and how many?
- The location of the fissure is next to the anus, or above or below the anus.
- The presence of any disease or other medical condition that causes fissures, such as: inflammatory bowel disease, anal cancer, syphilis, tuberculosis, suppressed immune system, HIV (AIDS) or Crohn’s disease, which can cause anal fissures and fistulas.
- Ensuring the presence or absence of any skin lump in the anus, as this is a sign that an anal fissure is chronic. Note that the skin lump may be incorrectly diagnosed as a hemorrhoid.
Fissure Treatment
- Laser therapy
- Advanced rectal slide therapy
- Material injection Treatment
- Fast
- security
- effective
- It can be performed under local anesthesia
- Drug therapy
Choosing the best and most appropriate treatment method for the incision requires an intra-anal pressure test (a simple, quick one-minute test) that helps the doctor choose the best treatment method.
Anal Fissure FAQ
I saw blood during defecation and it was dark red in color. Does this mean that there is an anal fissure?
I had a momentary pain during the intense pressure when defecating, but I did not feel any other pain later except for a slight continuous pain but very likely, is it possible for it to heal on its own?
I have an incision whose symptoms are clear, I had it yesterday, but I did not understand what is the treatment of the incision with gel-like, so how can the wound be closed with gel-like?
I think I have an incision and will go to the doctor, but I wanted to know if laser treatment is available in the clinic that I am going to visit, and is it available to you?
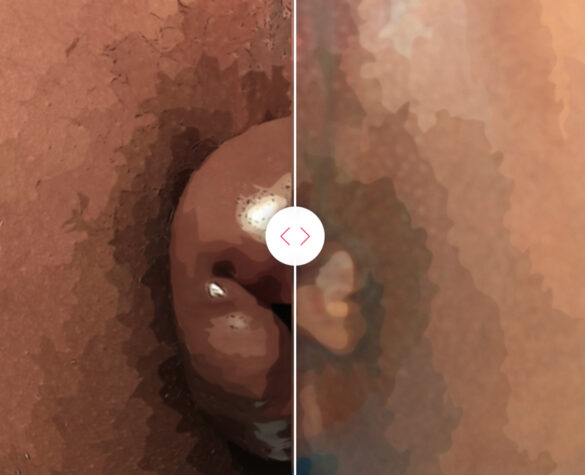
Fissure Cases
Patients who previously lived suffering from Hemorrhoid, Fissure, Pilonidal Sinus, Fistulas and received treatment at the hands of Dr. Khaldoon, we list to you what they suffered from the symptoms and the treatment that was provided may be of benefit.